“Mental health” and “mental illness” are health states at the opposite ends of a continuum. Even among mental health professionals, there are no agreed upon points on the continuum at which a “situation” becomes a “problem” or a “problem” becomes an “illness.” As the U.S. Surgeon General observes, “[t]here can be no doubt that an individual with schizophrenia is seriously ill, but for other mental health conditions such as depression or attention-deficit/hyperactivity disorder, the signs and symptoms exist on a continuum and there is no bright line separating health from illness, distress from disease.”
To further complicate matters, conditions may be called mental illnesses in some classification systems, but not in others – for example Attention Deficit/Hyperactivity Disorder is categorized variously as a mental illness or a learning disorder.
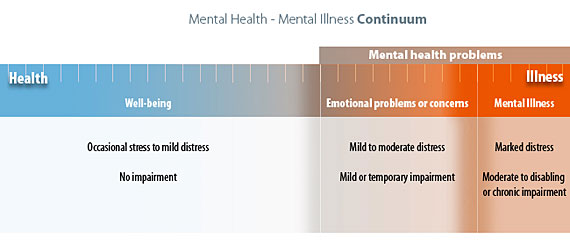
The Mental Health-Mental Illness Continuum
To establish a common language for this training, it is necessary to simplify and agree on terminology. For clarity, we have developed a diagram of the mental health-mental illness continuum employing the terms we use in this training.
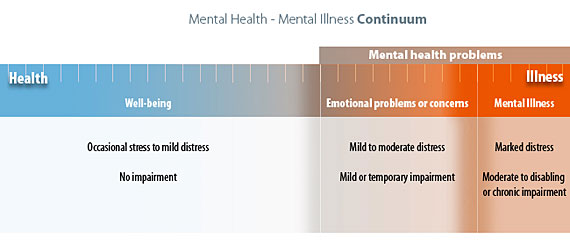
Along the continuum are three major mental health states in which individuals can be located at various times in their lives.
Well-being: At the “healthy” end of the continuum are individuals experiencing well-being, a state of good mental and emotional health. These individuals may experience stress and discomfort resulting from occasional problems of everyday life, but they experience no impairments to daily functioning.
All other individuals, for whom problems are more serious or prolonged, and for whom coping becomes progressively more difficult, are described as having “mental health problems.” Within this range are 2 categories of mental health conditions
Emotional problems or concerns: For individuals experiencing “emotional problems”, discomfort has risen to the level of distress accompanied by the beginning of impairments in functioning (e.g. insomnia, lack of concentration or loss of appetite). As the level of distress increases, individuals may seek professional counseling; those positioned at the right hand margin might be given diagnoses such as “situational” depression or “general anxiety”, indicating disorders with mild or temporary impairment. Some individuals with Attention Deficit Disorder who experience mild but long term impairment may also be found in this group.
Mental Illness: “Emotional problems” are raised to the level of “illness” by increase in distress and level of impairment. Located at the right end of the continuum, “mental illness” is characterized by alterations in thinking, mood, or behavior. Mental illnesses include relatively common disorders such as depression and anxiety as well as major disorders such as schizophrenia. Individuals with these disorders typically experience chronic or long-term impairments that range from moderate to disabling in nature.
As indicated by the continuum, mental health problems are common: we all experience problems in daily living at the milder end of the continuum; and at some point in our lives, we are likely to experience emotional problems or concerns. Mental illness, though less common, is nevertheless a frequent occurrence. It is estimated that approximately one in five Americans will personally experience a mental illness in their lifetime. This figure may, in fact, be low because mental illness, especially depression, is often associated with chronic physical illnesses such as diabetes, heart disease, hypertension and asthma, and is often not counted in epidemiological statistics when these conditions co-exist.
Mental health problems can affect anyone, regardless of age, culture, race, gender, ethnicity, economic status or location. However, the U.S. Department of Health and Human Services reports that while the prevalence of disorders is similar across races and ethnic groups, racial and ethnic minorities collectively experience greater disability from mental illness than do whites. This is because they receive less care and a poorer quality of care, circumstances associated with higher rates of poverty and lack of culturally sensitive services, not because their illnesses are inherently more severe or prevalent.